3 Reasons Why You Should Cultivate Endothelial Cells Under Flow
ibidi Blog | May 4, 2022 | Tina Freisinger, ibidi GmbH
In this blog article, we will discuss the reasons why it is essential to investigate endothelial cells (ECs) under flow conditions. The simulation of blood flow and the resulting mechanical force (shear stress) mimics the in vivo -like situation in blood vessels. Consequently, flow assays allow a physiologically more relevant investigation of endothelial cells and cardiovascular diseases compared to static cell culture experiments.
Background
ECs are an essential component of all blood vessels. They line the entire luminal surface of these vessels and function as permeability barriers between the vessel wall and the blood (Fig.1). Therefore, they are responsible for vascular homeostasis.
ECs play an essential role in regulating the vascular function in response to mechanical stimuli in both healthy and diseased states. One of their main tasks is to maintain the barrier function of the endothelium to regulate the exchange of blood with the underlying tissue by controlling, for example, the vascular permeability, leukocyte transmigration, and the vessel's mechanical stability.
In the living organism, ECs are permanently subjected to the mechanical stimulus of shear stress (Fig 1B). The circulation of blood generates this shear stress which has a crucial impact on the cells.
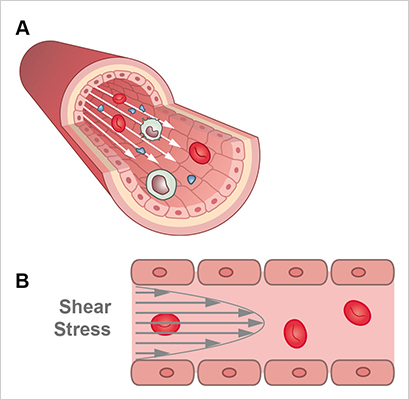
Fig. 1. Schematic depiction of a blood vessel lined with endothelial cells (A) and blood-fluid derived wall shear stress (B).
ECs are exposed to different types and degrees of shear stress, depending on the location and type of vessel or tissue. For example, venous cells are subjected to relatively low blood pressure and shear stress, whereas ECs in arteries endure high pressure and higher shear stress (Fig. 2).
In the straight sections of the arteries, blood flow is primarily laminar and unidirectional (small arteries), or laminar pulsatile (in large arterial vessels), whereas in branches or curvatures, the flow pattern can be nonuniform and disturbed. Disturbed or turbulent flow is often associated with a higher risk of the formation of atherosclerotic plaques.
It seems evident that these forces caused by fluid flow have a fundamental impact on the biology of ECs. In the following, we elaborate on why ECs should be cultivated under physiological shear stress rather than under static conditions.
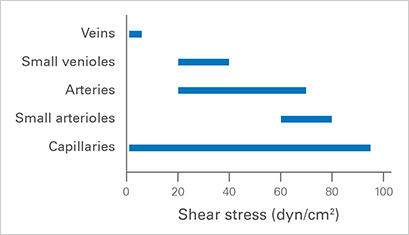
Fig. 2. Shear stress values in different human vessel types. Values derived from studies by BJ Ballerman et al., Kidney Internatl, 1998 and AM Malek et al., JAMA, 1999.
ibidi Flow Calculator
Simple calculation tool
for your flow experiments
1. Shear Stress Influences Cell Signaling and Gene Expression
Shear stress plays a crucial role in proper endothelial cell function by activating signaling cascades and gene expression involved in important biological processes (Fig. 3).
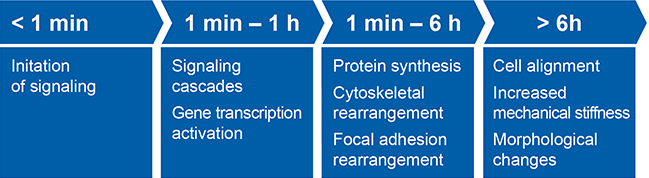
Fig. 3: Shear stress induced cellular changes. Adapted from PF Davies, Physiological Reviews, 1995.
The mechanical stimulus generated on endothelial cells by the fluid flow is sensed by mechanosensors located in the cell wall, such ion channels, the cytoskeleton, tyrosine kinase receptors, caveolae, G proteins, and cell-matrix (Integrins) cell-cell junction molecules. These mechanical stimuli trigger signaling cascades which are then transduced to the nucleus to activate transcription factors and gene expression. Subsequently, gene expression leads to protein expression and the activation of cellular functions such as remodeling of the endothelial cell structure or cell migration (Fig. 4).
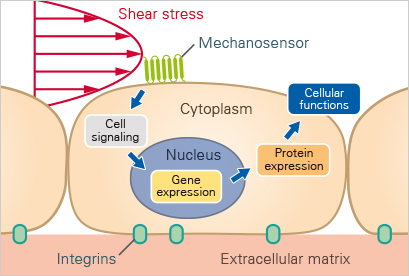
Fig. 4 Schematic diagram (adapted from Chien et al. 2007) showing the downstream effects of shear-stress induced mechanotransduction.
2. Shear Stress Influences Cell Morphology, Cell Structure, and Organization
The morphological impact of shear stress exposure becomes visually apparent even after a short period of cultivating endothelial cells under flow. In contrast to static cell culture, cells start to orient in the direction of the flow, and a rearrangement of the cytoskeleton takes place with actin fibers aligning in the direction of the flow (Figure 5). In addition, stress fibers and the mechanical stiffness of the cells increase.
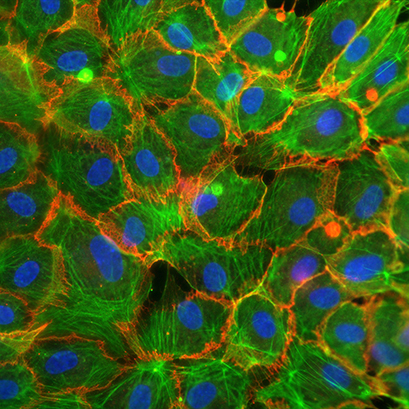
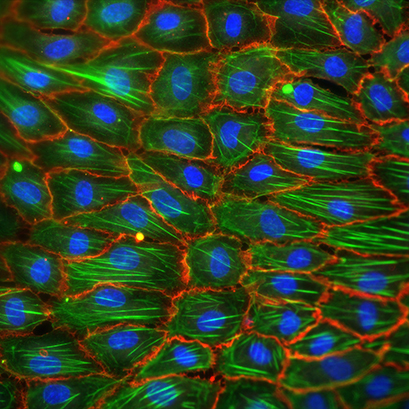
Fig. 5: Fluorescence microscopy of Human Umbilical Vein Endothelial Cells (HUVECs). Cells were cultivated for 72h with the ibidi Pump system under static (left) and flow conditions at 10 dyn/cm² (right). Afterwards, the cells were fixed and stained. Green: Actin, red = VE-Cadherin, blue = DAPI.
3. Shear Stress Influences Cell Function and Behavior
Shear stress induces changes in morphology, leading to cell function and behavior changes. The cytoskeleton acts as a transmitter of the mechanical stimuli into biochemical signaling processes, which then lead to changes in the cell proliferation, migration, and the macromolecular permeability of the cells. Moreover, it has been shown that shear stress influences the functionality of endothelial cells by regulating the cell barrier and cell-to-cell contacts as well as the micromotion of the cells (Fig 6.)
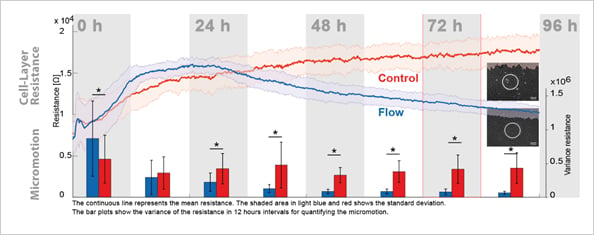
Fig. 6:
Impedance Micromotion decreases under flow conditions, as seen by the variance of the resistance signal. Shear stress: 10 dyn/cm2.
If you are interested in learning more about shear stress and cell culture under flow:
The Cell Culture Under Flow Application Site offers detailed information on:
- Biological implications of shear stress
- How to plan and set up a cell culture under flow experiment
- Flow types
- Experimental examples.
References:
- Chiu JJ, Chien S. Effects of disturbed flow on vascular endothelium: pathophysiological basis and clinical perspectives. Physiol Rev . 2011;91(1):327-387. doi:10.1152/physrev.00047.2009 Read article
- Mussbacher M, Schossleitner K, Kral-Pointner JB, Salzmann M, Schrammel A, Schmid JA. More than Just a Monolayer: the Multifaceted Role of Endothelial Cells in the Pathophysiology of Atherosclerosis. Curr Atheroscler Rep. 2022 Apr 11. doi: 10.1007/s11883-022-01023-9. Read article
- Malek AM, Alper SL, Izumo S. Hemodynamic shear stress and its role in atherosclerosis. JAMA. 199 Dec 1; 282(21):2035-42. doi: 10.1001Tjama.282.21.2035. Read article
- Chien S. Mechanotransduction and endothelial cell homeostasis: the wisdom of the cell. Am J Physiol Heart Circ Physiol. 2007 Mar;292(3):H1209-24. doi: 10.1152/ajpheart.01047.2006. Read article
- Li H, Zhou WY, Xia YY, Zhang JX. Endothelial Mechanosensors for Atheroprone and Atheroprotective Shear Stress Signals. J Inflamm Res . 2022;15:1771-1783. 10.2147/JIR.S355158. Read article
- Davies PF. Flow-mediated endothelial mechanotransduction. Physiol Rev. 1995 Jul;75(3):519-60. doi: 10.1152/physrev.1995.75.3.519. Read article
- Li YS, Haga JH, Chien S. Molecular basis of the effects of shear stress on vascular endothelial cells. J Biomech. 2005 Oct;38(10):1949-71. doi: 10.1016/j.jbiomech.2004.09.030. Read article
- Braddock M, Schwachtgen JL, Houston P, Dickson MC, Lee MJ, Campbell CJ. Fluid Shear Stress Modulation of Gene Expression in Endothelial Cells. News Physiol Sci. 1998 Oct;13:241-246. doi: 10.1152/physiologyonline.1998.13.5.241. Read article
- Tsaryk R, Yucel N, Leonard EV, Diaz N, Bondareva O, Odenthal-Schnittler M, Arany Z, Vaquerizas JM, Schnittler H, Siekmann AF. Shear stress switches the association of endothelial enhancers from ETV/ETS to KLF transcription factor binding sites. Sci Rep. 2022 Mar 21;12(1):4795. doi: 10.1038/s41598-022-08645-8. Read article
- Chien S, Li S, Shyy YJ. Effects of mechanical forces on signal transduction and gene expression in endothelial cells. Hypertension. 1998 Jan;31(1 Pt 2):162-9. doi: 10.1161/01.hyp.31.1.162. Read article
 (5)
(5)  (0)
(0)